According to the Congressional Budget Office, a federal agency that provides budget and economic information to Congress, it can take up to 10 years and cost more than $3 billion to produce and release a new drug into the market. This inefficiency is attributed to the reliance on traditional methods such as animal testing and Petri dish models to assess drug efficacy and safety. However, the problem lies in the fact that though these methods have been used for decades, they cannot mimic the effects of these drugs on humans because these traditional models don’t contain human cells! This is where the Organs-on-Chips technology plays a vital role in speeding up drug discovery, revolutionizing the pharmaceutical industry, and paving the pathway for personalized medicine.
Traditional Methods VS Organ Chip Technology
The two traditional methods for drug discovery include animal testing and in vitro models using Petri dishes. Various animal species, including mice, rats, rabbits, birds, and even dogs, are utilized in animal testing due to their biological similarities to humans. However, the fact is that in addition to the high cost, the lack of sufficient congruence between animal models and human diseases makes this ancient practice an inefficient one. Although the latter course of using in vitro models does utilize human tissue to explore the toxicities of the drug, it is not in the right environment. The human body is a complicated three-dimensional space different from the cell-cultured models. The limitations of these traditional systems are creating a large gap between predictions in preclinical testing and what happens in humans during clinical trials, slowing the entire process and making it more expensive.
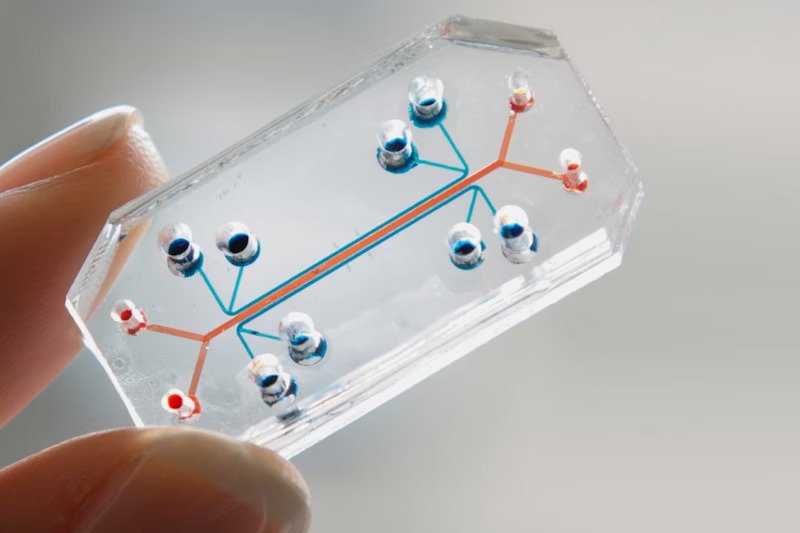
The organ chip technology differs like this: the microchip is composed of a porous membrane with the organ tissue on one side and the capillary cells on the other, mimicking the original structure. The membrane, surrounded by vacuum channels, enables organ movement. The fascinating fact is that this model recreates the tissue and the organ’s responses. For example, if a lung tissue placed on one of these tissues has a bacteria function, it uses the surrounding capillaries to send chemical signals to alert the immune system. This mechanism makes detecting the responses of diseases and drugs during drug discovery faster, cheaper, and more efficient without directly involving animals or humans. In fact, during the COVID-19 pandemic, Emulate, a biotechnology company that first commercialized Organs-on-Chips technology, signed a collaborative agreement with the FDA to use this technology to test the safety of the COVID vaccines. More recently, FDA stated that it intends to focus on reducing animal testing and increasing the use of cutting-edge technologies like the organ chip to develop safe drugs.
Applications of Use
Aside from the technology’s benefits in the pharmaceutical industry, it can be utilized in several other industries. For instance, to analyze the effects of a cosmetic product on the skin, you can apply the product to a small piece of skin tissue placed on a microchip. This method can help create safe cosmetic products and enable cruelty-free cosmetics, a more ethical approach to medical testing. Similarly, the human tissue can be placed on the microchip to test the effects of chemicals we’re exposed to in everyday life (detergent, soap, cleaning liquid, etc.), contributing to the development of safer consumer products. Moreover, the organ-on-a-chip model can be used to investigate the impacts of radiation on different organs by pinpointing the mutation sites, helping scientists develop mitigation strategies for these radiation-induced diseases. The organ chip technology holds significant potential in addressing the challenges posed by bioterrorism and assisting scientists in finding solutions for those caused by such acts. These examples highlight the versatility of organ chip technology across various industries, where it can contribute to the development of innovative solutions and advancements.
Personalized Medicine
Imagine having a specific treatment plan for a disease specifically tailored just for you to match your unique body. That’s what organ chip technology aims to provide. Although we’re all very similar, we’re all also not. We each have our unique genetic profile that determines the slight differences in immune responses, which is why the engineers of this technology are working towards displaying more than one organ at a time on the chip, moving toward the replication of the entire body. Then they can take a sample of an individual’s distinct stem cells and analyze it on the chip to customize a personalized treatment plan based on the observed effects.
The clinical trial of Vatine et al. of Cedars-Sinai Medical Center can be an example. Researchers of this study used stem cells from a patient with Huntington’s disease to model barrier permeability in the Blood-Brain Barrier. They used the specific stem cells because this patient had a mutation that was directly causing this disease. Therefore, they needed to analyze the patient’s specific stem cells to develop a treatment plan. A similar procedure can help form a personalized treatment plan for other diseases, especially genetic disorders.
As we look to the future, organ-on-a-chip technology holds immense promise for advancing our understanding of human biology, transforming the process of discovering new drugs, and ultimately improving patient outcomes. With these microchip devices, personalized medicine may become a reality, where therapies are customized to match individual patients’ genetic profiles. The ongoing advancement and use of organ-on-a-chip technology will play a crucial role in shaping the future of biomedical research and opening the door for safer, more effective drugs that can significantly impact global healthcare.
Works Cited
“Emulate Signs Collaborative Agreement With the FDA to Apply Lung-Chip to Evaluate Safety of COVID-19 Vaccines and Protective Immunity Against SARS-CoV-2.” BioSpace, 29 Oct. 2020, www.biospace.com/article/releases/emulate-signs-collaborative-agreement-with-the-fda-to-apply-lung-chip-to-evaluate-safety-of-covid-19-vaccines-and-protective-immunity-against-sars-cov-2.
Moskowitz, Jake, DVM PhD. “Organ-on-a-Chip: A Personalized Approach to ≪Em≫in Vitro≪/Em≫ Modeling.” Today’s Clinical Lab, June 2023, www.clinicallab.com/trends/precision-medicine/organ-on-a-chip-a-personalized-approach-to-em-in-vitro-em-modeling-26307.
Nuwer, Rachel. “US Agency Seeks to Phase Out Animal Testing.” Nature, Nature Portfolio, Nov. 2022, https://doi.org/10.1038/d41586-022-03569-9.
Risueño, Iván, et al. “Skin-on-a-chip Models: General Overview and Future Perspectives.” National Library of Medicine, vol. 5, no. 3, Sept. 2021, p. 030901. https://doi.org/10.1063/5.0046376.
TED. “Geraldine Hamilton: Body Parts on a Chip.” YouTube, 3 Dec. 2013, www.youtube.com/watch?v=CpkXmtJOH84.
Vatine, Gad D., et al. “Human iPSC-Derived Blood-Brain Barrier Chips Enable Disease Modeling and Personalized Medicine Applications.” Cell Stem Cell, vol. 24, no. 6, Elsevier BV, June 2019, pp. 995-1005.e6. https://doi.org/10.1016/j.stem.2019.05.011.
Wyss Institute at Harvard University. “Human Organs-on-Chips.” Wyss Institute at Harvard University, n.d., https://wyss.harvard.edu/technology/human-organs-on-chips/.